January 2014
HISTORY
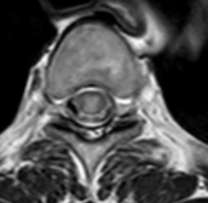
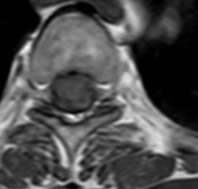
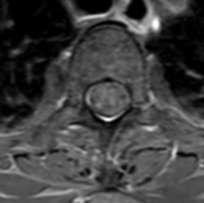
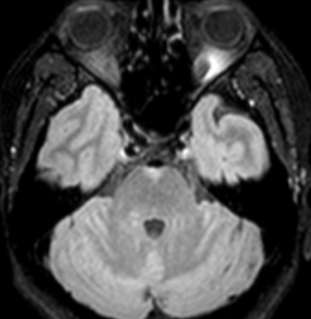
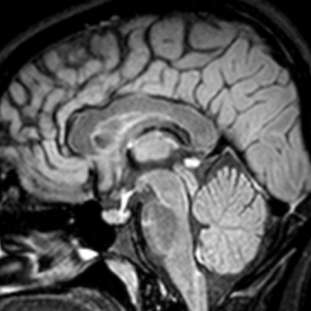
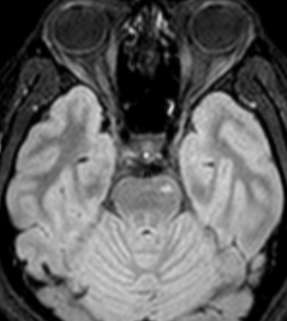
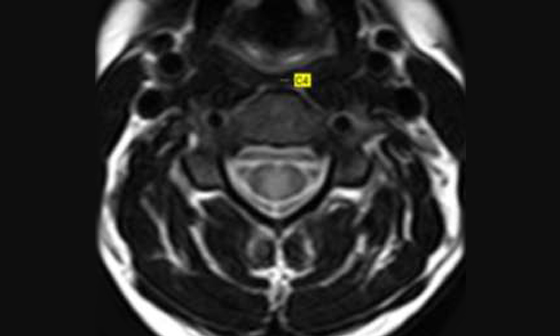
CASE 1:
- 30 year old female patient
- Presented with gradual onset tingling numbness in whole body with weakness of both upper limbs
- Underwent MRI cervical spine at another centre in November 2013 which was reported as cord neoplasm and biopsy was advised
- Second opinion on MRI study raised possibility of inflammatory etiology
- Patient responded to treatment with Injection methyl predisolone with persistent tingling numbness in both upper limbs
- Follow up imaging was done at our centre in Jan 2014
- Screening of brain was also performe Readmore