July-August Clinical Newsletter
Dear Doctor,
It gives me immense pleasure to present, the first edition of this bimonthly newsletter in collaboration with Philips Healthcare, showcasing few interesting clinical cases done at our center.
STAR Imaging and Research Centre is Pune's premier diagnostic institute which has brought to the city its FIRST 3 Tesla MRI, which is the best in the country. We also house state-of-the-art MULTISLICE CT scanner.
The very purpose of this new letter is to make clinical and academic contribution and to help all of us learn from experience. We look forward to your encouraging support in this endeavor.
Dr. Ashish Atre
Case 1:
(Courtesy Dr. Vinay Thorat&Star Imaging &Research Centre)
Clinical Presentation:
67 years old gentleman was detected to have cirrhosis. His AFP values were not elevated. He was referred for MR.
 Fig 1a and b: T2W axial image (a) shows focal lesion appearing hypointense with an eccentric hyperintense area. The focal lesion appears heterogenously bright on TI W (b)out of phase gradient echo axial images.
Fig 1a and b: T2W axial image (a) shows focal lesion appearing hypointense with an eccentric hyperintense area. The focal lesion appears heterogenously bright on TI W (b)out of phase gradient echo axial images.
 Fig 2 a and b: Post contrast dynamic T1 W arterial (a) and portal venous phase(b) axial images show the T1hyperintense area enhancing on the arterial phase & washing out on the venous phase.
Fig 2 a and b: Post contrast dynamic T1 W arterial (a) and portal venous phase(b) axial images show the T1hyperintense area enhancing on the arterial phase & washing out on the venous phase.
Take home Imaging Message: MR is more sensitive as compared to CT for detection of HCC is a cirrhotic liver. T2 dark & T1 bright lesions on MR are due to paramagnetic effects secondary to iron deposition in dysplastic nodules.T2 hyperintensity in a dark nodule raises a possibility of malignant transformation to HCC in a dysplastic nodule. Hypervascularity in the arterial phase and washout in the venous phase adds to the diagnostic confidence.
REFERENCE - MR Imaging of Hepatocellular Carcinoma in the Cirrhotic Liver: Challenges and Controversies, Jonathon M.Willatt, et al May 2008 Radiology, 2 4 7, 31 1-330.
Case 2:
(Courtesy Dr. Sudhir Kothari & Star Imaging & Research Centre)
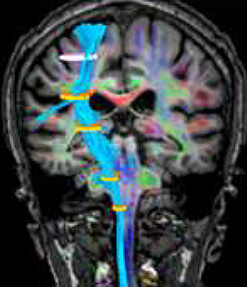
Middle aged man presented with first episode of convulsion & was referred for MRI brain
MR revealed hyperperfused SOL in the left frontal region abutting the falx. Spectroscopy revealed increased choline and reduced creatinine & NAA. Perfusion and spectroscopic abnormality were restricted to enhancing portion of lesion with surrounding tissues showing return to normality.
Possibility of metastases was raised with differential diagnosis of meningioma.
 Fig 1 a and b: T2W axial (a) and T1 past contrast axial (b) images shows a well defined lesion with perilesional edema & post contrast enhancement
Fig 1 a and b: T2W axial (a) and T1 past contrast axial (b) images shows a well defined lesion with perilesional edema & post contrast enhancement

 Fig 2 a and b: Perfusion map (a) and multivoxel MR spectroscopy (b) images shows high perfusion restricted to the tumor (a). The MR spectroscopy images reveal grossly elevated choline with marked reduction of (NAA & creatinine (b).
Fig 2 a and b: Perfusion map (a) and multivoxel MR spectroscopy (b) images shows high perfusion restricted to the tumor (a). The MR spectroscopy images reveal grossly elevated choline with marked reduction of (NAA & creatinine (b).
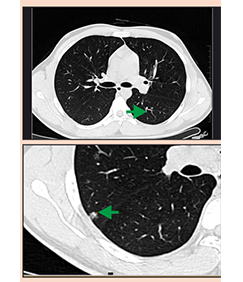
Patient underwent CT thorax the next day revealing left upper lobe mass, with histology revealing Primary Bronchogenic Carcinoma.

Take home imaging message: Perfusion MRI and Multi-voxel MR Spectroscopy may help in differentiating primary v/s metastatic intracranial tumours. This is due to the fact that primary brain tumours are infiltrative by nature and perfusion as well as spectroscopy abnormality extend beyond the apparent lesion margins. This is not seen in metastatic brain tumours.
REFERENCE - High grade gliomas & solitary metastases: Differentiation by using perfusion & proton MR spectroscopy MR imaging. Meng Law et a//, Radiology: March 2002, 222:715-721
Case 3:
(Courtesy Dr. Sudhir Kothari & Star Imaging & Research Centre)
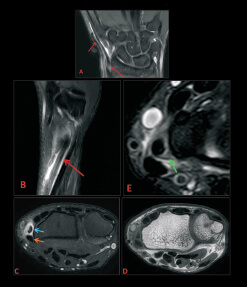
49 year old gentleman with history of swelling over the lateral aspect of right knee joint since 4 months & foot drop since 2 months. Clinical examination revealed right peroneal neuropathy.

 Fig 1 a and b: T2W coronal (a) and sagittal (b) images shows a well defined lesion in the peroneus longus muscle. It appears hyperintense with a dark rim on T2Wls.
Fig 1 a and b: T2W coronal (a) and sagittal (b) images shows a well defined lesion in the peroneus longus muscle. It appears hyperintense with a dark rim on T2Wls.

 Fig 2 a and b: T2W axial (a) and STIR axial (b) images shows intraneural cyst in (a). The sections below the level of knee joint shows changes of denervation atrophy in the proximal extensor digitorum longus and tibialis anterior muscles and patchy areas involvement of the peroneus longus muscle.
Fig 2 a and b: T2W axial (a) and STIR axial (b) images shows intraneural cyst in (a). The sections below the level of knee joint shows changes of denervation atrophy in the proximal extensor digitorum longus and tibialis anterior muscles and patchy areas involvement of the peroneus longus muscle.
Take home Imaging Message: Peroneal ganglion cysts are relatively unusual findings on MRI. Compressive neuropathy of the common peroneal nerve or its branches may occur:
MRI is the modality of choice to delineate the anatomic boundaries of the lesion. Communication with superior T/F joint may be demonstrated. Compression of peroneal nerve or extension of cyst within the peroneal nerve is best assessed by MRI. The sequelae of denervation will be seen as hyperintensity of the muscles on STIR images and fatty change on T1WIs.
REFERENCES: REFERENCES: 1. Illahi OA et al Prevalence of ganglion cysts originating from the proximal tibiofibular joint: A magnetic resonance imaging study. Arthroscopy. 2003 Feb;19(2):150-3 2. McCarthy CL et al. The MRI appearance of cystic lesions around the knee. Skeletal Radiol. 2004 Apr;33(4): 187-209. Epub 2004 Feb 27
Case 4:
(Courtesy Dr. Amol Talaulikar& Star Imaging & Research Centre)
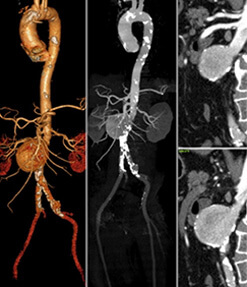
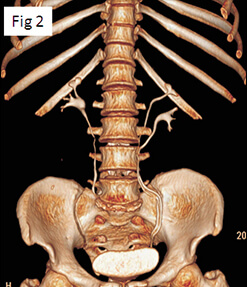
Elderly man had undergone radical prostatectomy for Ca prostate 2 years ago has now presented with rising PSA levels. (Previously undetectable PSA)

 Fig 1 a and b: T2W axial (a) and T1 dynamic post contrast axial (b) images shows small nodule in right para-urethral location in the prostatic fossa. This nodule enhances brilliantly on post-contrast study.
Fig 1 a and b: T2W axial (a) and T1 dynamic post contrast axial (b) images shows small nodule in right para-urethral location in the prostatic fossa. This nodule enhances brilliantly on post-contrast study.