Head and Neck Imaging at Star
VOL. II • MAY-JUNE 2015 CLINICAL NEWSLETTER
Head and Neck Radiology is a challenging imaging subspeciality which is slowly but surely gaining recognition in India. It includes imaging pathologies involving the extracranial head and neck / face region. The Head and Neck Imaging division at Star performs and interprets scans pertaining to diseases of the skull base, ear, orbits, sinuses, upper airway and neck spaces as well as the oral cavity, lip and jaws etc through a comprehensive imaging package which incorporates high frequency ultrasonography, and dedicated high resolution CT and MRI scans using specialized equipment / coils. The division specializes in complete ENT imaging, biologic imaging of head neck cancers with emphasis on pre-operative work-up of potential cochlear implant candidates.imaging of cholesteatoma, CSF leaks.sleep disorders, and T-M joint pathologies.Ultrasound guided FNACs of subcentimeter thyroid nodules and cervical masses/ lymph nodes as well as elastography is also performed at STAR.
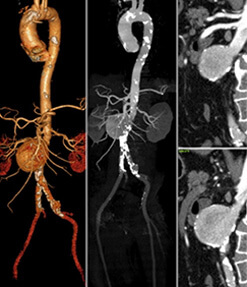
HEAD AND NECK CANCERS
Case1: Lipomatous synovial sarcoma of the retropharyngeal space in a child.
An IO year old male child presented with dysphagia, breathlessness and disturbed sleep.

 Key points:
Key points:
- 1. Head and neck region synovial sarcomas are rare tumors in the pediatric population
- 2. Occur due to malignant degeneration of pluripotential primitive mesenchymal cells which can be located at a location remote from synovial tissue. These tumors appear to originate primarily from the paravertebral connective tissue spaces, presenting later as retropharyngeal or parapharyngeal masses, the hypopharynx being the commonest site in the head and neck.
- 3. Three histological variants have been described: the classical biphasic type, the monophasic fibrous type and the monophasic epithelial type.
- 4. None of the synovial sarcomas described to date in medical literature have reported the presence of adipose tissue within the tumor.
- 5. A recently concluded research study at ST AR showed that intra-tumoral ADC values > 1.2 x I 0•3 mm2 / sec indicates greater chances of the lesion being malignant and ADC values < 1.2 x I 0- 3 mm2 / sec indicates greater chances of the lesion being benign.
Case 2: Non-Hodgkins Lymphoma (NHL) ofthe temporal bones.
A 50 year old male presented with gradually increasing right ear pain, right occipital swelling and left facial palsy.
 Key points:
Key points:
- 1. Lymphomas of the temporal bone are rare tumors: Hodgkins disease, B-cell non-Hodgkin lymphoma and mycosis fungoides.
- 2. Primary lymphoma: from mucosa of mastoid antrum / tympanum / tympanic orifice of the Eustachian tube (these regions have a layer of lymphoid tissue deep to the epithelium).
- 3. Differential diagnosis: Wegner's, sarcoidosis,fungal disease.
- 4. Imaging:
- CT: Irregular osteolytic permeative bone destruction with associated masses.
- MRI: Intermediate to low signal on TI and T2W sequences with post-contrast enhancement. Useful in differentiating tumor from adjacent inflammatory / retro-obstructive changes.
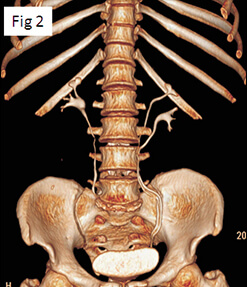
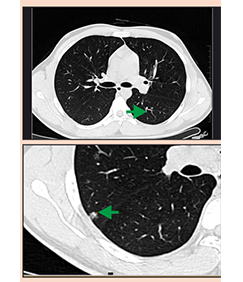
Case 3: Giant Cell Tumor (GCT) of the maxillary sinus.
A 42 year old female presented with swelling and pain over right maxillary region since 3 months gradually increasing in size.
 Key points:
Key points:
- 1. GCTof the head and neck: rare, approximately 2% of all GCTs
- 2. Usually benign, but can be primarily malignant or undergo malignant transformation andalso metastasize.
- 3. Imaging:
- CT: multilocularmultiseptate appearance, can show presence of multiple fluid levels.
- MRI: usually have fairly low signal intensity on all sequences and enhance on contrast administration.
CONGENITAL ANOMALIES OF THE INNER EAR: INCOMPLETE PARTITION DEFECTS (TYPE 1, 2, 3)
All patients presented with severe to profound bilateral hearing loss in the age group of I I months to 3 years.
Case 1: Incomplete Partition Defect Type I with Type 2ACVNDHCB

Case 2: Incomplete Partition Defect Type 2 with dilated vestibular aqueduct (Mondini'sdeformity ) and normal cochleo-vestibular nerve

Case 3: Incomplete Partition Defect Type 3 (X-linked deafness) and normal cochleo-vestibular nerves on both sides.

Key points:
- 1. Type I: Cystic cochlea and vestibule. No scala or modiolus. Wide communication with IAC.
- 2. Type II: Normal basal turn with scala and base of modiolus. Fused apical and middle without scala and modiolus Mondini's deformity: Type II with dilated vestibule and enlarged vestibular aqueduct.
- 3. Type III: Normal external cochlea with a 'cork-screw appearance’.lntactscala with absent mod iol us.
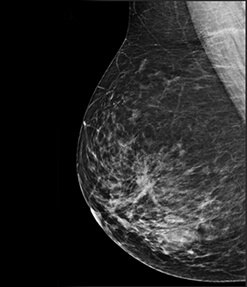
MR IMAGING FOR CHOLESTEATOMA VIS GRANULATION AND SCAR TISSUE
Case I: Right primary acquired cholestetoma.
23 year old male patient withhistory of right sided conductive hearing loss and purulent discharge.

Case 2: Post-operative granulation and scar tissue.
30 year old female patient was operated for right sided cholesteatoma one year back. She presented with symptoms of headache, persistent right ear discharge and conductive hearing loss on right side.
 Key points:
Key points:
- 1.HRCT and MR combination with emphasis on Single Shot-Non Echoplanar Turbo Spin Echo Diffusion Weighted Imaging is the ideal combination for diagnosing/ rulingout presence of cholesteatoma.
- 2. Basis of imaging protocol: Cholesteatomas mimic epidermoid cysts on MR irrespective of location in the temporal band exhibits diffusion rest rictio n.
- 3. MRI is useful in the diagnosis of cholesteatoma and also for differentiating cholesteatoma from granulation tissue/ post-operative scar tissue.
- 4. This imaging protocol may o bviate the need for 'second- look' surgery.
INVESTIGATING CSF LEAKS
Case I: CT Cisternography.
32 year old male patient with history of right sided spontaneous CSF rhinorrhoea.

Case 2:44 year old female patient with history of left sided spontaneous CSF rhino r rhoea.
 Key points:
Key points:
- 1. Plain non-contrast enhanced HRCT of the paranasal sinuses is the initial investigation in cases of CSF rhinorrhoea to identify focal bony defects in the skull base.
- 2. Non-contrast MR cisternography using surface coils provides high resolution images in all planesand in conjunction with the HRCT images, is a useful non-invasive technique to demonstrate most of the CSF leaks which can then be addressed endoscopically and sealed.
- 3. In special circumstances CT cisternography is performed after intrathecal injection of non-ionic contrast medium under all aseptic precautio ns. Cotton pledgets which are placed in both nasal cavities (medial and lateral to the middle turbinates) are scanned separately before and after the intrathecal injection of contrast medium.
- 4. Use of low volume (< I ml) intrathecal Gadolinium is more sensitive (nearly I 00%) in detection of CSF leaks, very useful for intermittent leaks as the contrast medium is visible for 24 hours after injection and has relatively less side effects of meningeal reactio n / headache as compared to the non-ionic watersolublecontrast medium currently being used for intrathecal injections.
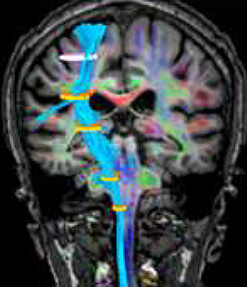
IMAGING FOR OBSTRUCTIVE SLEEP APNOEA SYNDROME
Case I :CT Cephalometry.
CT Cephafometric measurements are made on the lateral scout view and six standard bony and so-tissue measurements are obtained:
MP-H distance: from the mandibular plane to the hyoid bone. The normal value is I 5.4 ± 3 mm.
PNS-U distance: from the posterior nasal spine to the tip of the uvula, which provides a measure of the length of the soft palate? The normal value is 34 ± 6 mm.
SP-max: maximum thickness of the so palate perpendicular to PNS-U.
SNA, SNB, and ANB angles: S is the midpoint of the self a, N is the nasion, and A is the deepest point on the premaxillary outer counter; B is the deepest point on the outer mandibular contour. The normal value of ANB angle is 2°; SNA angle is 82°; and SNB angle is 80°.

Case 2 :Dynamic MRI studies.
 Key points:
Key points:
- I. Obstructive sleep apnea syndrome (OSAS) is a common form of sleep-disordered breathing characterized by repetitive episodes of partial or complete upper airway obstruction.
- II. 2. The etiology of OSAS includes abnormalities in both the physiology and anatomy of the airway and associated facial structures. The upper airway lumen is narrower in patients with obstructive sleep apnea syndrome (OSAS) than normal subjects because of fat infiltration, the weight of the soft tissue of the neck, or reduced pharyngeal muscle tone.
- III. The average number of episodes of apnea and hypopnea per hour of sleep is referred to as the apnea-hypopnea index or AHI. An AHI of 5 -29 represented mild/moderate OSAS and an AHI≥30 represents severe OSAS.
- IV. 4. Imaging patients with OSAS includes CT cephalometry studies to investigate the craniofacial architecture of patients with OSAS, in which measurements and abnormalities of the craniofacial structures are well documented. This is complimented with dynamic MRI studies in awake and sleep state which provides information about airway cross-sectional area and site of collapse, when performed in different phases of respiration.
- V. Cross-sectional areas of the airway measured at the level of velopharynx, base of tongue and hyoid bone and six standard cephalometric measurements are made on the lateral CT scout view of the head.
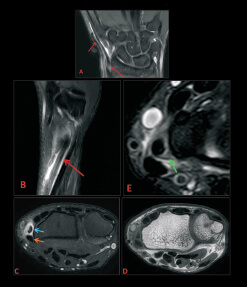
IMAGING INTERNAL DERANGEMENTS OF THE T-M JOINT
Case I: Normal sagittal image of the left T-M joint in closed and open mouth position.

Case 2: Bilateral internal derangement of the left T-M joints.
 Key points:
Key points:
- I. Indications for MR examination of the T-M joints:
a. Internal Derangements (ID)
- All kinds of disc displacement
- Disc adhesions
- Degenerative disorders and avascular necrosis
- Differentiation between disc displacement and pathology of the surrounding tissue
b. Inflammatory Disorders
c. Mobility / Symmetry Issues
- Comparison of the motion of both jaws (hyperlaxity)
- Luxation of the mandibular condyle
- Maxillomandibular asymmetry - 2. Causes of Internal Derangements (ID) of the T-M joints:
- Acute macrotrauma: external blow,mandibular whiplash, jaw hyperextension.
- Chronic macrotrauma: low-grade trauma over a long period (bruxism.DJD)
- Developmental & acquired defects: hypo/hyperplastic condyles, asymmetric facial dysplasias, endocrine and nutritional disorders, tumors and infections. - 3. Imaging protocols:
- PDW, T2 fat suppressed sagittal and PDW coronal sequences in close mouth position.
- PDW,T2 fat suppressed sagittal sequence in open mouth position.
- Dynamic sequences obtained during opening of mouth.
- STIR axial images of the upper neck. - 4. What the radiologist needs to report: - Articular disc - Morphology, position, displacement, adhesions. (‘stuck disc')
- Joint effusion and synovitis.
- Osseous changes
- Osteoarthritis - Degenerative Joint Disease
- Miscellaneous intra-articular causes of ID
- Extra-articular mimics of ID
MR SIALOGRAPHY
MR sialography using special surface coils with 3T scanners and dedicated sequences is a highly successful technique for noninvasive visualization of the ductal system of major salivary glands, useful in diagnosing sialolithiasis with sialectasis and accompanying ductal changes in sialadenitis.
Case 2: Bilateral internal derangement of the left T-M joints.

The main advantages of MR sialography are:
- I. Non-invasive technique as compared to conventional sialography.
- II. Lack of ionizing radiation as we are examining more of a relatively young population with benign salivary glandular /ductal diseases.
- III.Can be performed in patients in the acute stage and also in patients with known reactions to iodinated contrast material.