Breast Imaging at Star
Dr. Aparna Atre
Breast Imaging
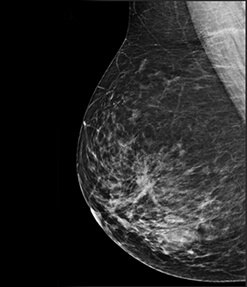
Breast cancer incidence is growing at an alarming rate all over the world. In India, the scenario happens to be no different with breast cancer incidence as high as 1 in every 22 females in the urban population. What is especially alarming in the Indian setting is the younger predilection for cancer (peak age incidence is 43 to 46 years as compared to the western peak of 53 to 56 years). In addition the preponderance of dense fibroglandular parenchyma seen in the Indian breasts reduces the sensitivity of the mammography evaluation.
To specifically address these issues related to Indian women a superior technology is required. We at STAR IMAGING are pleased to announce the launch of the state of the art FULL FIELD DIGITAL MAMMOGRAM along with 3 D TOMOSYNTHESIS as well as the whole gamut of BIOPSY ATTACHMENTS.
Since all these technologies are new and revolutionary we will start by briefly outlining about them.
FULL FIELD DIGITAL MAMMOGRAPHY
FFDM uses specially designed digital detectors along with advanced computer technology to produce images which are displayed and evaluated on high resolution monitors.
There is 'direct conversion' at the level of the image production which preserves image sharpness and produces images of exceptional quality – a prerequisite for detecting early breast cancer.
There is also a reduction in radiation dose by 30 to 50 % with FFDM machines.
This is in sharp contrast to the machines currently prevalent in the market and called 'DIGITAL' but are actually offline reading machines where early breast cancers can often be missed.
3 D MAMMOGRAM OR TOMOSYNTHESIS
The FFDM system provides us with a platform to perform TOMOSYNTHESIS where at the same setting the Xray tube moves in an arc over the breast and captures multiple low dose images. These are then reconstructed by the computer to produce 1 mm thin slices.
So instead of viewing the breast in a flat 2D image we view the finer details of the breast by scrolling through the stack of images 1 mm at a time.
This machine comes equipped with a special technology that allows us to reconstitute 2D images just by taking low does tomoexposures. (the entire radiation exposure for this type of study would be less than one film exposure in currently available systems used in the city)
This helps us to easily do the mammography in young patientswithout the worry of radiation risks. It also helps us to add information in already done half-hearted studies without subjecting the patient to additional radiation.
Dr.Varsha Hardas INTERVENTIONS POSSIBLE FOR BREAST LESIONS
Until now ifmicrocalcifications suspicious for early breast cancer were detected it was an uphill task to further evaluate them for a histopathological diagnosis.
With the advanced vacuum assisted biopsy system these microcalcifications can be accurately targeted under stereotactic guidance. With the help of Vacuum a fairly good chunk of tissue can be easily removed and sent for confirmation.
Non palpable small lesions under 2 cm in size can be removed non surgically with vacuum assistance. This is especially of help in non-palpable lesions which can be approached with the imaging technique they are best seen in (mammo, ultrasound or MRI). This lesion removal is done as an office procedure with the patient walking home within an hour.
In addition image guided procedures such as FNAC, core biopsy, aspirations, drainage procedures and wire localizations for the breast are being routinely performed.
BREAST ULTRASOUND
To counter the problem of dense breasts which is prevalent in the Indian population, a supplementary sonomammogram is also performed for all mammography patients. A dedicated high frequency transducer with a foot plate modified for breast tissue is available to perform these studies on the high end Phillips IU 22 machine. The frequency of this probe can go as high as 17 mHZ making it an ideal platform to evaluate the superficial and small breast structures such as the ducts with confidence. In addition it comes with a fully loaded breast elastography package. Elastography evaluates the breast lesions on the basis of their tissue stiffness and codes them with colour graphs and actual values (EQ values). This helps us to differentiate benign versus malignanat lesions with more comfort and also obviates the need for biopsies at times.
BREAST MRI
To complete the gamut of breast imaging solutions the centre has a wide bore Phillips Ingenia 3T MRI unit with a dedicated breast coil to perform breast imaging.
Breast MRI is commonly used to diagnose the entire extent of disease process and presence of additional cancer foci in a diagnosed case of breast cancer. It is also useful in post-operative patients to differentiate scar tissue versus recurrence. It is also of benefit as an additional screening tool in young women and those with genetic mutations positive for breast cancer. It is also a modality of choice in imaging patients with breast implants.
Case 1
Courtesy:Dr.Pranjali Gadgil
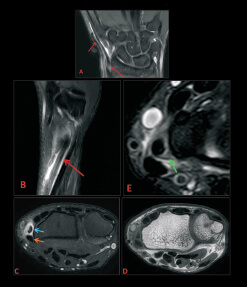
A 39 YEAR OLD LADY PRESENTED WITH RIGHT SIDED HAEMORRHAGIC NIPPLE DISCHARGE.


Review of Literature
The terminal ductal lobular unit of the breast is an important structure because most invasive cancers as well as ductal carcinoma in situ (DCIS) along with many benign processes arise from the TDLU.
Most calcifications in the breast form either within the terminal ducts (intraductal calcifications) or within the acini (lobular calcifications).
Intraductal calcifications are suspicious of malignancy and are classified as BI-RADS 4 or 5. These calcifications are calcified cellular debris or secretions within the intraductal lumen. The uneven calcification of the cellular debris explains the fragmentation and irregular contours of the calcifications. These calcifications are extremely variable in size, density and form (i.e. pleomorphic from the Greek pleion 'more' and morphe 'form'). Sometimes they form a complete cast of the ductal lumen called as linear casting with a fine linear or branching form and distribution.
Imaging Pearls
FFDM along with digital tomosynthesis forms the mainstay to diagnose breast microcalcifications. Distribution and morphology are the two main considerations while evaluating microcalcifications. A linear and segmental branching pattern would definitely indicate a ductal distribution immediately raising our suspicions.
Presence of linear casting and pleomorphic calcifications would confirm our suspicion of malignant calcifications. These suspicious microcalcifications are best tackled with stereotactic vacuum assisted biopsy removal which helps us to get histopathological confimation of the disease process.
Case 2
Courtesy:Dr.Aarti Nimkar
A 53 YEAR OLD LADY CAME WITH A PALPABLE LUMP IN THE RIGHT BREAST.

Review of Literature
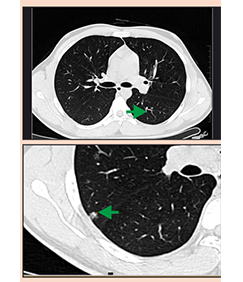
Digital breast tomosynthesis provides us an invaluable tool to pick up smaller additional foci of breast cancer.
Small irregular or spiculated lesions are picked up only by DBT especially if these are merging with the surrounding breast tissues On DBT the well circumsribed margins are also well delineated giving the radiologist greater confidence in calling a lesion benign.
Multi focal breast cancer masses refers to two or more individual breast cancers diagnosed at the same time within the same quadrant of the breast and necessarily less than 5 cm apart.
It has an impact on patient management as multifocal breast cancers tend to have more nodal involvement, higher chances of local recurrence and poorer prognosis as compared to unifocal disease.
Irregular spiculated masses form one of the classical presentations of breast malignancy, with the lesion directly classifying as BIRADS 5.
Imaging Pearls
Here the cyst presents as a “red herring”. It is merely the palpable abnormality which has directed the patient to the doctor. The 2 D images alert us to the fact there is coexistent cancer in this breast. However the use of DBT helped us find 3 foci of cancer and confirm multifocal disease.
Case 3
Courtesy : Dr. Sanjay Deshmukh
59 YEAR OLD LADY ALREADY UNDERWENT A MASTECTOMY FOR THE RIGHT BREAST. NOW COMPLAINING OF DISCHARGE FROM THE OPPOSITE BREAST.
Imaging Pearls
Patients with a know history of breast cancer are at double the risk as compared to the general population for recurrence of the opposite side. These patients therefore are on routine follow up. A neodensityon serial follow up scans should immediately warrant attention. Presence of spiculations in this neodensity seen on the FFDM as well as TOMO images definitely raise our suspicion level.

Case 4
Courtesy:Dr. Shona Nag, Dr.Rathi
TWO PATIENTS IN THE AGE GROUP OF 45 TO 50 YEARS. ONE PATIENT HAD A LUMPISH FEELING IN THE LEFT BREAST WHILE THE OTHER ONE CAME FOR A ROTUINE SCREEENING EVALUATION.






Review of Literature
Invasive carcinoma distorts the interfaces between fat and normal breast parenchyma due to the desmoplastic response of host tissue due malignancy. In the fatty breast this presents no diagnostic dilemma, since this is seen as typical spiculations as we saw in the previous case. However in dense breasts the tumor mass can be so obscured by adjacent benign tissues so as to be invisible. In this case just an area of focal architectural distortion presents as the only indication of malignancy.
Tomosynthesis serves as an ideal tool in this situation. By eliminating the problem of tissue overlap it allows us to see the tissues in 1 mm slice intervals making it possible to seen the typical spiculations evenin extremely dense breasts helping us diagnose breast cancers indense breasts with greater confidence.
Imaging Pearls
In the first case the only abnormality seen in the 2D images is the obvious asymmetry seen in left breast on the MLO views. The TOMO images clearly show the spiculated lesion confirming our supicions.
In the second case the architectural distortion is obvious on the 2D images in the superoouetr aspect of the left breast.
The spiculated margins of this lesion causing the architectural distortion are well seen on the tomo slices.
Thus it is important to remember that subtle architectral distortion and asymmetry will probably present us the first clue to the underlying abnormality. Tomosynthesis is a great tool helping us confirm these subtle abnormalities with ease.
Case 5:
Courtesy:Dr.Sujai Hegde
SCREEN DETECTED, NON PALPABLE LESIONS.

Clinical presentation:Routine screening. Positive Family history. Sister recently detected of Breast Cancer. Mother treated for breast cancer in the past.
BI-RADS IV, nonpalpable 9mm lesion was core – biopsied under usgguidance for this patient. Histopathology is benign.
Howeverexcision is advised for the same for complete evaluation, and wirelocalization with surgical excision or vaccum assisted complete excision with marker deployment can be offered to this patient.
Imaging Pearls:Usg is extremely useful in young, pregnant patients, and in inflammatory conditions for diagnostic as well as theurapeutic options. It is also very useful for close follow ups.
Usg with high resolution linear probes can be a very useful adjunct to mammography in older patients to characterize the lesions andincreases the sensitivity and specificity of the study.
Usg guided FNAC and Core biopsy for histopathology is very accurate, simple and useful diagnostic procedure done routinely in our center with great yield.
Clinically non-palpable lesion assessment and diagnostic test have to be done under usg guidance only.
Usg guided pre-operative wire localizations can be done for excision of small non-palpable lesions. Complete Excision of small clinically non-palpable benign lesions can be done with Vacuum Assisted Biopsy with USG guidance, very accurately .It is FDA Approved. It is an OPD procedure done under Local Anesthesia, leaves no scar and also has all the tissue for accurate histopathology evaluation.
MRI BREAST: POST – OPERATIVE BREAST EVALUATION
Case 1
Courtesy :Dr.Minish Jain
Clinical presentation:A 48 yr old woman with history of Breast conservative surgery for the left breast complains of nodularity in the operative bed.

Case 2
Courtesy:Dr.Shekhar Kulkarni
Clinical presentation:38yr old woman with h/o BCS in the left breast for routine screening. Mammography inconclusive as she has extremely dense breast parenchyma.

Case 3
Courtesy:Dr.Bhushan Zade
Clinical presentation:60yr old lady with history of Right Breast conservative surgery, now complains of pain and fullness in the operative bed.

Case 4
Courtesy:Dr. Shona Nag
Clinical presentation:50yr old lady with post BCT status left breast with heaviness in the left breast and at the operative site.

Review of Literature:
With Mammography and Sonography the assessment of residual disease has limitations, due to the postoperative changes, granulation tissue formation, distortions, hematoma, seroma, and fibrosis in and around the operative bed. All these can mimic residual disease. All these also affect the clinical examination findings, and it is difficult to assess the operative bed on follow ups. Residual disease that is untreated may eventually manifest itself as Recurrence, early or late. It may be argued that radiation may take care of this, but not all, and we don't know which will be and which will not, especially if there is no pre-operative assessment and there is a large bulky residual disease left behind.
MRI can also assess complications like hematoma, seroma, infection in the operative bed accurately with higher sensitivity and specificity as compared to other modalities.
Imaging Pearls:MRI is very sensitive in assessing bulky residual lesion in a post lumpectomy patient. It is also very useful in assessing Recurrence in patients treated with BCT.
It has high NPV. It means a negative study confirms no Residual disease or Recurrence. It has high sensitivity in differentiating scar tissue from Residual disease / Recurrence due to enhancement in the tumor and noenhancement in the fibrous tissue of scar.
MRI is very helpful in guiding the surgeon for planning Re – Excision surgery when needed.
MRI BREAST: PRE-OPERATIVE EVALUATION
Case 1
Courtesy:Dr.Anupama Mane
Clinical presentation:46yr old lady with vague palpable nodularity in the left breast. Mammography study done outside showed very dense breast and was Negative.
USG showed a small suspicious lesion in the left breast. FNAC of clinically palpable nodularity in the upper quadrant proved to be grade II Lobular Carcinoma.
MRI was done to know the exact extent of the disease and also for contralateral breast assessment.

Case 2
Courtesy:Dr.Anupama Mane
Clinical presentation:45yr old lady with painful small lump in the right breast UIQ posterior in location, and had close approximation to pectoral muscle on Mammography and Sonography.

Case 3
Courtesy:Dr.Anupama Mane
Clinical presentation:40 yr old lady with small breast and a large BiradsV lesion in the left breast UIQ. Pectoral involvement could not be assessed on Mammography.
Review of Literature
Accurate Assessment of extent of disease is essential for planning appropriate optimal treatment for women with breast cancer. Detection of Multicentric or Multifocal disease can guide the surgeon to plan the treatment accordingly. Involvement of pectoral muscle, chest wall and or skin indicate the need for surgical excision of these areas. Identification of cancer in contralateral breast indicates the need to address that too.
In cases of Lobular carcinoma MRI is especially very crucial for preoperative assessment as Mammography can be falsely negative. Lobular cancer have higher frequency of Multicentricity and bilaterality.
MRI is known to detect cancer that is not palpable and not evident on Mammography and Sonography and provides more accurate assessment of the tumor size. All these contribute for better surgical outcome.

Imaging Pearls
MRI should be done routinely for pre-operative assessment to know the exact extent of disease when Mammography and Sonography fail to do so, especially in patients with extensively dense breast parenchyma. In patients of biopsy proven Lobular Carcinoma, and in assessing patients with Implants, for Breast Cancer MRI is very useful. Chest wall, Pectoral muscle, and skin involvement can be assessedvery well with MRI. This information affects surgical planning.
USG – BREAST: INFLAMMATORY LESIONS
Case 1 and Case 2
Courtesy:Dr.Aarti Shirali

Case 3
Courtesy:Dr.Sanjay Rayate

Case 4
Courtesy: Dr. A. Mane
All these young patients presented with typical symptoms of pain, swelling, redness and tenderness, fever.

Review of Literature
USG is the gold standard in evaluating inflammatory changes in young patients. Mammography has a limited role in such cases, and especially if the patient is below 35yrs, then it should not be done.
High Resolution Linear probes are essential for evaluation of breast lesions on USG. Usg involves no Compression and no Radiation, and so is very useful in Pregnant, young patients, and in Evaluation of Inflammatory Conditions .It is easy to follow up these patients by USG .
USG guided diagnostic aspiration for culture sensitivity can be easily done, so that appropriate treatment can be offered.
Therapeutic aspirations can be done routinely under USG guidance, and can be repeated if and when necessary and follow up can be done till complete resolution is attained.
Surgical procedures can be avoided in young patients there by avoiding associated issues like scars, anesthesia, damage of the ductal system etc.